Blogs
Items filtered by date: August 2024
Tuesday, 27 August 2024 00:00
Sesamoiditis
Sesamoiditis is a condition in which the sesamoid bones in the forefoot become inflamed from physical activity. Sesamoid bones are bones that are not connected to other bones but are located in tendons or muscle. Two of these sesamoid bones are very small and located on the underside of the foot near the big toe. Athletes such as runners, baseball and football players, and dancers are likely to experience sesamoiditis. Those with high arched feet, flat feet, or runners who run on the ball of their foot are also prone to suffer from sesamoiditis.
Symptoms include pain or throbbing on the ball of the foot near the big toe. The pain generally starts with a mild throbbing but gradually builds up to shooting pain. Bruising, swelling, and redness are possible, but in most cases, these symptoms are not present. However, moving the big toe can result in pain and difficulty.
To conduct a diagnosis, the podiatrist will examine the ball of the foot and big toe. They will look for any outliers and check the movement of the toe. X-rays will be taken to rule out any other conditions and ensure that it is sesamoiditis.
Treatment for sesamoiditis is generally mild and includes rest, anti-inflammatory and pain medication, and ice treatments to deal with the swelling and pain. Orthotics may be needed with people who have flat or high arched feet to relieve pressure off the bones. In some cases the toe will be taped and immobilized to allow healing. The podiatrist may also decide to use a steroid injection to help with swelling as well. If you have sesamoiditis, you shouldn’t engage in any intensive activity, as it may inflame the area and worsen your pain. If the sesamoid bone has fractured, surgery may be required to remove the sesamoid bone.
If you are suffering from sesamoiditis or are experiencing symptoms similar to sesamoiditis, you should stop all physical activity that puts strain on the area. Furthermore you should see a podiatrist for a diagnosis to see if you have sesamoiditis.
Tuesday, 27 August 2024 00:00
Identifying and Treating Sesamoiditis
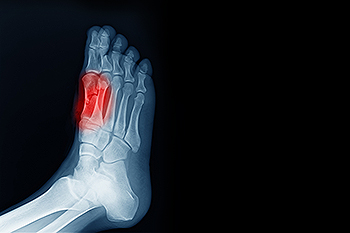
Sesamoiditis is an irritation of the two sesamoid bones that are located beneath the first metatarsal head of the foot. It leads to pain that can be particularly bothersome during activities like walking or running. These tiny bones, each about the size of a kernel of corn, play a significant role in foot movement. They can become painful due to trauma, foot structure changes, or repetitive stress. Sesamoiditis is often seen in dancers, runners, and those who frequently wear high heels. Symptoms can include localized pain beneath the big toe, swelling, and tenderness that worsens with pressure. Diagnosis typically involves a clinical evaluation by a podiatrist, sometimes supported by imaging tests to rule out fractures or other conditions. Treatment focuses on reducing pressure on the sesamoids through footwear modifications, including supportive shoes and custom orthotics. If you have pain under the big toe, it may be related to the sesamoid bones, and it is suggested that you schedule an appointment with a podiatrist for an exam and treatment.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact one of the podiatrists of JE Foot & Ankle Associates. Our doctors will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact one of our offices located in Fleming Island and Palm Coast, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Tuesday, 20 August 2024 00:00
Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Tuesday, 20 August 2024 00:00
Stages of Toenail Fungus

Toenail fungus progresses through distinct stages, each requiring timely intervention. In the earliest stage, the nail may appear slightly discolored, usually yellow or white, with minimal discomfort. Without treatment, the condition advances to the moderate stage, where the nail becomes thicker and more discolored, and may develop a crumbly texture. This stage often involves some pain or discomfort. If untreated, toenail fungus can reach an advanced stage, causing severe thickening, distortion, and detachment of the nail from the nail bed. This stage can lead to significant pain and difficulty walking. In the chronic stage, the infection is longstanding and difficult to treat, potentially leading to permanent damage. If you notice the beginning stages of toenail fungus, it is suggested that you consult a podiatrist who can offer you effective treatment options which may prevent advancing to later stages.
For more information about treatment, contact one of the podiatrists of JE Foot & Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact one of our offices located in Fleming Island and Palm Coast, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Tuesday, 13 August 2024 00:00
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Tuesday, 13 August 2024 00:00
Open Wounds on the Feet
 Open wounds on the feet are injuries where the skin is broken, exposing underlying tissues. These wounds can vary in type, including cuts, abrasions, lacerations, punctures, and ulcers. Cuts and lacerations often result from sharp objects, while abrasions are usually caused by friction or scraping against rough surfaces. Puncture wounds occur from stepping on pointed objects. Ulcers are typically associated with poor circulation, diabetes, or prolonged pressure. Open wounds on the feet require prompt and appropriate treatment to prevent infection and promote healing. Initial care involves cleaning the wound thoroughly with mild soap and water, followed by applying an antiseptic. Keeping the wound covered with a sterile bandage and changing it regularly is critical. If you have an open foot wound, it is strongly suggested that you schedule an appointment with a podiatrist who may need to debride it, prescribe antibiotics, and in some cases, stitch up the wound or do surgery to ensure proper healing and prevent complications.
Open wounds on the feet are injuries where the skin is broken, exposing underlying tissues. These wounds can vary in type, including cuts, abrasions, lacerations, punctures, and ulcers. Cuts and lacerations often result from sharp objects, while abrasions are usually caused by friction or scraping against rough surfaces. Puncture wounds occur from stepping on pointed objects. Ulcers are typically associated with poor circulation, diabetes, or prolonged pressure. Open wounds on the feet require prompt and appropriate treatment to prevent infection and promote healing. Initial care involves cleaning the wound thoroughly with mild soap and water, followed by applying an antiseptic. Keeping the wound covered with a sterile bandage and changing it regularly is critical. If you have an open foot wound, it is strongly suggested that you schedule an appointment with a podiatrist who may need to debride it, prescribe antibiotics, and in some cases, stitch up the wound or do surgery to ensure proper healing and prevent complications.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of the podiatrists from JE Foot & Ankle Associates. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Fleming Island and Palm Coast, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Tuesday, 06 August 2024 00:00
Causes, Symptoms, and Treatment of Poor Blood Circulation in the Feet
Poor blood circulation in the feet and legs is often caused by peripheral artery disease (PAD), which is usually the result of a buildup of plaque in the arteries. Plaque buildup, or atherosclerosis, can be the result of excess calcium and cholesterol in the bloodstream. This restricts how much blood can flow through arteries. Reduced blood flow to a certain area of the body severely limits the amount of oxygen and nutrients that part of the body receives. This leads to degeneration in the muscles and other tissues. Sometimes, poor blood circulation in the feet and legs can be caused by other conditions, such as the damaging or inflammation of blood vessels, known as vasculitis.
The lack of oxygen and nutrients caused by poor blood circulation can restrict muscle growth and development, as well as cause muscle pain and cramps, weakness, and stiffness. Other common symptoms include numbness in the legs and feet, skin discoloration in the affected limbs, slower nail and hair growth, and erectile dysfunction in men. In more severe cases of PAD, pain can be present even when a person isn't exercising, and may range from mildly uncomfortable to completely debilitating.
Poor blood circulation in the feet and legs is more common in those who are overweight or obese, have diabetes, high blood pressure, high cholesterol, who smoke, or who have a family history of PAD or related conditions such as a heart attack, stroke, etc. Diabetes and smoking place a person at greatest risk for developing poor blood circulation, although advanced age, over 50, can also increase risk.
If you are experiencing poor blood circulation in the feet and legs caused by PAD, it is important to make changes to your lifestyle in order to reduce your risk of experiencing a heart attack or stroke caused by this condition. If you smoke, quit completely. This will increase the amount of oxygen in your bloodstream. Exercising and reducing the saturated fats in your diet. Saturated fats come from fatty meats, fried foods, whole milk, etc., can make a difference in improving blood circulation in feet. It is also important to avoid developing influenza and to carefully control your blood sugar if you have diabetes.
Your doctor may recommend combining lifestyle changes with a prescription medication regimen to improve blood circulation. The most commonly-used medications for PAD are called statins and work by blocking the amount of enzymes in your body that produce cholesterol. They are known by the brand names Zocor, Lipitor, Crestor, and others.
Tuesday, 06 August 2024 00:00
Improving Poor Foot Circulation

Poor foot circulation can lead to discomfort and potentially serious health issues. To improve foot circulation, start by incorporating regular physical activity into your routine, such as walking or swimming, to stimulate blood flow. Elevating your feet when sitting or lying down can also help to reduce swelling and promote circulation. Avoid crossing your legs for long periods, as this can restrict blood flow. Massage therapy can be beneficial for increasing circulation and reducing muscle tension. Wearing compression socks or stockings can improve circulation by helping veins and muscles move blood more effectively. Staying hydrated and maintaining a balanced diet can help to support overall vascular health. Lastly, quitting smoking and managing conditions like diabetes and high blood pressure can further improve blood flow to the feet. If you have poor foot circulation, it is suggested that you contact a podiatrist who can help you manage this condition by guiding you toward additional effective relief strategies.
While poor circulation itself isn’t a condition; it is a symptom of another underlying health condition you may have. If you have any concerns with poor circulation in your feet contact one of the podiatrists of JE Foot & Ankle Associates. Our doctors will treat your foot and ankle needs.
Poor Circulation in the Feet
Peripheral artery disease (PAD) can potentially lead to poor circulation in the lower extremities. PAD is a condition that causes the blood vessels and arteries to narrow. In a linked condition called atherosclerosis, the arteries stiffen up due to a buildup of plaque in the arteries and blood vessels. These two conditions can cause a decrease in the amount of blood that flows to your extremities, therefore resulting in pain.
Symptoms
Some of the most common symptoms of poor circulation are:
- Numbness
- Tingling
- Throbbing or stinging pain in limbs
- Pain
- Muscle Cramps
Treatment for poor circulation often depends on the underlying condition that causes it. Methods for treatment may include insulin for diabetes, special exercise programs, surgery for varicose veins, or compression socks for swollen legs.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact one of our offices located in Fleming Island and Palm Coast, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Friday, 02 August 2024 00:00
Why Live with Pain and Numbness in Your Feet?
Blog Archives
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019

